Media
HKU Scientists Discover the UTE Disc Sign as a New Low Back Pain Imaging Biomarker Providing Insight into Degenerative Disc Disease of the Spine
16 Aug 2017
(Back from left) Dr Dino Samartzis, Associate Professor; Dr Jason Cheung Pui-yin, Clinical Assistant Professor; Ms Cora Bow Hing-yee, Senior Research Assistant; and Professor Keith Luk Dip-kei, Tam Sai-Kit Professor in Spine Surgery and Chair Professor, Department of Orthopaedics and Traumatology, Li Ka Shing Faculty of Medicine, HKU.
(Front from left) Dr Uruj Zehra, Post-doctoral Fellow of Department of Orthopaedics and Traumatology; and Dr Henry Pang, Master of Research in Medicine student, Li Ka Shing Faculty of Medicine, HKU.
Low back pain (LBP) is the world’s most disabling condition, affecting up to 80% of the population. Such pain is associated with tremendous socioeconomic and health-care consequences. For the past 30 years, the “conventional” T2-weighted magnetic resonance imaging (MRI) has been broadly used to diagnose LBP; however, it is not highly sensitive and reliable, and as such may not be useful to identify the cause and treatment of LBP. This study, led by the Department of Orthopaedics and Traumatology, Li Ka Shing Faculty of Medicine, The University of Hong Kong (HKU), is the first to report that the Ultra-Short Time-to-Echo Disc Sign (UDS) was found to be significantly related to degenerative spine changes, LBP and disability in comparison to conventional MRI imaging. The research has been published in the international journal Spine this month (August 2017 issue).
Low back pain
Although LBP is a multifactorial complex disorder, several studies have noted lumbar disc degeneration as a risk factor. MRI is considered the gold-standard among imaging options to assess soft-tissues of the human body, in particular the intervertebral discs of the spine, to understand what may lead and cause LBP. For the past 30 years, “conventional” T2-weighted MRI has been used to assess the spinal discs and spine degeneration. This current imaging is not highly sensitive and reliable, and as such may not be useful to “predict” future LBP episodes secondary to disc degeneration. Such shortcomings may provide a rationale as to why it is common to find symptomatic individuals with seemingly normal (i.e. non-degenerated) discs and asymptomatic individuals with degenerative disc changes on conventional MRI. This may account as to why proper diagnosis of LBP and identification of pain mechanisms are questionable, outcomes of LBP treatments are often tenuous and have been criticised, and prognostication potential of various pain and disability dimensions as well as management options have drawbacks. Thus, such limitations have led to increased health-care costs with often unsatisfactory patient outcomes.
In the past decade, various novel MRI technologies have been developed in an effort to address more sensitive measures to assess spine degeneration. One such imaging technology is Ultra-Short Time-to-Echo (UTE) MRI. UTE MRI assesses MRI signal from short T2 components that are not detected on conventional T2-weighted MRI. It can be performed on any MRI machine and takes approximately 15-20 minutes to scan the lumbar spine of one individual, which is similar in time as conventional MRI sequences. Utilising UTE MRI, the research team has identified a new disc biomarker, called the UTE Disc Sign (UDS), and its clinical importance.
Significance of the study
This study is the first to report the finding and clinical relevance in humans of the UDS on MRI. The UDS is a novel, reliable and simple MRI biomarker to assess the intervertebral lumbar discs, its relationship with other findings of spine degeneration, and its implications upon LBP and disability. The UDS was found to be significantly related to degenerative spine changes, LBP and disability in comparison to conventional MRI imaging. The UDS may serve as a new imaging marker that may have potential implications in diagnostic, therapeutic and prognostic platforms in patients presenting with LBP or possibly be able to predict the development and severity of pain. The UDS may also shed light upon the pathomechanism of spinal disc changes that may become painful.
According to the lead investigator, Dr Dino Samartzis, Associate Professor of Department of Orthopaedics and Traumatology, Li Ka Shing Faculty of Medicine, HKU, “For the past 30 years, it has been argued time and time again that findings on conventional MRI or imaging that are commonly used worldwide are not strongly related to LBP or disability. Many clinicians and scientists have often questioned the practical use of having patients undergo such costly conventional imaging to determine the source of pain and that degenerative disc findings are commonplace among individuals who are also not in pain. Our study provides the ‘missing link’ between imaging findings of the spine and the development of LBP and disability.”
Dr Samartzis further noted that “Using UTE MRI, this has allowed us an opportunity to identify ‘hidden’ degenerative disc findings in an easy, quick and reliable fashion that helps us understand what’s going on within the spinal discs much better than ever before. This has also led us to understand why someone may develop LBP and if the pain may indeed have its ‘origins’ within the disc.” Dr Samartzis further added that “This new imaging technology and the assessment of the UDS may supplement conventional MRI, therefore providing a larger snapshot into a patient’s spine degeneration and pain profiles, thereby allowing clinicians to develop more personalised and precise management options to improve patient outcomes. This certainly represents a new leap forward in the visualization of the spinal discs and perhaps pain.”
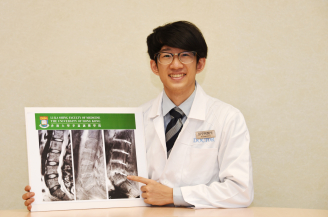
Dr Henry Pang, Master of Research in Medicine student, Li Ka Shing Faculty of Medicine, HKU and first author of the study, further noted that “Among various MRI sequences, UTE MRI is the only sequence so far in our study that showed definite correlation between back pain, disability and degenerative disc changes. At the same time, as our study group unveils the previously hidden pathologies in traditional MRI, these findings may promote further understanding in the pathologies and therapies for low back pain and lumbar degeneration.”
Research method
One hundred and eight (108) Southern Chinese participants were recruited (mean age: 52 years, equal number of male and female subjects). T2-weighted MRI was used to assess disc degeneration and other phenotypes, and T1-rho MRI values represented quantitative proteoglycan content (i.e. water) of the disc. UDS was detected on UTE as a hyper- or hypo-intense band across a disc. The cumulative number of UDS levels represented a UDS score, whereas summated degenerated scores of lumbar levels via T2-weighted MRI represented a cumulative disc degeneration score. Subject demographics, LBP every day (chronic) in the past year and disability profiles (Oswestry Disability Index: ODI) were obtained.
Research findings
The UDS was noted in 39.8% subjects, of which 61.4% occurred at the lower lumbar levels. Subjects with UDS had significantly more disc degeneration and levels with pathologic changes of the vertebral bodies (i.e. Modic changes). Based on disc levels, a higher prevalence of disc degeneration and disc bulges/protrusions, Modic changes and spondylolisthesis (i.e. slippage of the vertebral body) were noted in UDS discs than non-UDS discs (p<0.05). T1-rho values were lower in UDS discs than non-UDS discs (p=0.022). The majority of UDS could not be detected on conventional T2-weighted MRI. The UDS score was significantly correlated with worse ODI scores (r=0.311; p=0.001) and pain (p=0.009), whereas T2-weighted cumulative disc degeneration score was not (ODI: r=0.13; p=0.19, LBP: p=0.127). 39.5% of UDS subjects who had multi-level involvement also had a higher prevalence of LBP (p<0.015), however this correlation was not found on T2-weighted MRI (p=0.53).
Moving forward
Future study plans are underway to identify what these UDS findings truly represent and how they contribute to the mechanism of LBP, as well as predicting future episodes of pain. Further initiatives are also being planned to address large-scale, prospective and multicenter international studies to further validate our findings, and assess the utility of the UDS on different clinical and research platforms.
About the research team
This study was done in collaboration between the Department of Orthopaedics and Traumatology, Li Ka Shing Faculty of Medicine, HKU and the Department of Radiology, University of Pennsylvania, Philadelphia, USA, the Department of Orthopaedics, Fourth Military Medical University, Xi’An, China, the Finnish Institute of Occupational Health, University of Oulu, Finland and the Department of Orthopedic Surgery, RUSH University Medical Center, Chicago, USA. The Hong Kong team was composed of Dr Dino Samartzis, Associate Professor of Department of Orthopaedics and Traumatology, Professor Kenneth Cheung Man-chee, Jessie Ho Professor in Spine Surgery, Clinical Professor and Head of Department of Orthopaedics and Traumatology, Professor Keith Luk Dip-kei, Tam Sai-Kit Professor in Spine Surgery and Chair Professor of Orthopaedic Surgery of Department of Orthopaedics and Traumatology, Dr Jason Cheung Pui-yin, Clinical Assistant Professor of Department of Orthopaedics and Traumatology, Dr Uruj Zehra, Post-doctoral Fellow of Department of Orthopaedics and Traumatology, Ms Cora Bow Hing-yee, PhD candidate of Department of Orthopaedics and Traumatology, as well as Dr Henry Pang, Master of Research in Medicine student, Li Ka Shing Faculty of Medicine, HKU.
Media enquiries
Please contact Li Ka Shing Faculty of Medicine of The University of Hong Kong by email (medkefa@hku.hk).
Dr Dino Samartzis, Associate Professor of Department of Orthopaedics and Traumatology, Li Ka Shing Faculty of Medicine, HKU points out that UTE MRI can identify “hidden” degenerative disc findings in an easy, quick and reliable fashion that helps us understand the pain may indeed have its ‘origins’ within the disc.
MRI of the lumbar spine of a subject with no chronic low back pain.
(Left) T2-weighted MRI noting multilevel disc degeneration and Modic changes.
(Right) Ultra-short time-to-echo (UTE) MRI noting no UTE disc sign (UDS).