Media
HKU discovers how SARS-CoV evades respiratory innate immunity to establish a systemic infection
28 Dec 2015
Although the Severe Acute Respiratory Syndrome Coronavirus (SARS-CoV) epidemic was successfully contained by July 2003, there remains serious concern regarding a recurrence of severe CoV-mediated disease. Indeed, an outbreak of Middle East Respiratory Syndrome coronavirus (MERS-CoV) occurred in South Korea from May 2015 to July 2015, leading to 186 cases infected and a death toll of 36. It is surprising that people’s knowledge of the innate immune defenses in the upper respiratory mucosa, in particular during acute SARS-CoV infection, remains rather limited. Researchers at AIDS Institute of Li Ka Shing Faculty of Medicine, The University of Hong Kong (HKU) have recently discovered how SARS-CoV evades respiratory innate immunity to establish a systemic infection in collaboration with scientists of the Chinese Academy of Medical Sciences (CAMS) and Tulane University in the United States.
After several years of research, the team discovered that SARS-CoV might hijack innate immune cells including monocytes/macrophages and the dendritic cells to facilitate viral transmission from the portal of entry to mucosa-associated lymph tissues and subsequent systemic infection. The findings highlighted the facts that while these innate immune cells contribute to viral clearance and immune response induction, they may also serve as shelters and vehicles, providing a mechanism for the virus to evade host defenses and to disseminate systemically. These results were recently published in the leading journal of the Immunology field, Mucosal Immunology.
Dr Li Liu, Research Assistant Professor of Department of Microbiology and the AIDS Institute at Li Ka Shing Faculty of Medicine, HKU, who primarily conducted the study, says, “Unraveling how upper airway mucosal exposure of SARS-CoV results in the establishment of infection and subsequent systemic virus dissemination is critical in understanding SARS pathogenesis and to identify key steps for the future prevention of related disease.”
Methodology
To investigate the early events of SARS-CoV infection, scientists of the AIDS Institute of Li Ka Shing Faculty of Medicine, HKU used the Chinese rhesus macaque model. They divided 15 Chinese rhesus macaques into four study groups. After pathogenic SARS-CoV challenges, samples of entire respiratory system were obtained for a comprehensive analysis at day 2, 3 and 7 post infection respectively. This allows the scientists to investigate the early immune cells upon SARS infection.
Research findings
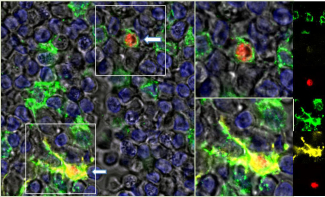
In human upper respiratory mucosal system, epithelium is the first-line natural barrier whereas the underneath innate immune cells act as the incoming pathogen. The epithelium serves as the defensive wall while the innate immune cells fight like soldiers inside the wall. When SARS-CoV infects mucosal epithelium directly, the innate immune cells become activated to clear the virus. They include monocytes/macrophages, dendritic cells and natural killer cells, etc. Monocytes/macrophages can engulf virus and virus-infected cells to clear infection. At the same time, dendritic cells can also engulf virus and virus-infected cells in order to capture antigen and stimulate adaptive immune response in mucosal associated lymphoid tissues.
Scientists found that SARS-CoV breaches the mucosal barrier by infecting the respiratory epithelium, mainly around the pharynx and larynx, and subsequently infects mucosal Langerhans cells (a type of dendritic cells) and resident macrophages. In the meantime, CD163+ and MAC387+ monocytes/macrophages are quickly recruited in droves by a chemotactic gradient from infected epithelium and tissue resident macrophages. However, these monocytes/macrophages are unlikely to be sufficient to eliminate the incoming viral attack, which allows Langerhans cells and monocytes/macrophages carrying the virus to migrate to the mucosal associated lymph tissues and draining lymph nodes via the afferent lymphatics. Once inside lymph nodes, CD163+ macrophages unexpectedly support productive viral replication upon differentiation into dendritic cells, which carry virus. Free virus and infected dendritic cells may infect or trans-infect new target cells in lymph respectively and then leave through the efferent lymphatics for systemic dissemination.
Dr Li Liu concluded, “This finding provides a clearer picture in understanding the mechanism how SARS-CoV evades respiratory innate immunity for viral seeding at the portal of entry and early systemic infection. Our findings will allow scientists to simulate the spread of SARS-CoV or other viruses alike in the upper respiratory tract in a more effective and accurate way. The study may also have important implications for developing strategies for early interventions and immunotherapy.”
Another key researcher of the study, Professor Zhiwei Chen, Professor of the AIDS Institute and Department of Microbiology of Li Ka Shing Faculty of Medicine, HKU says, “The study for the first time revealed the complex role of monocyte/macrophage during early dissemination events of SARS-CoV infection, which is impossible to study in humans.”
About the research team
The study is jointly conducted by the AIDS Institute and Department of Microbiology of Li Ka Shing Faculty of Medicine, HKU, Chinese Academy of Medical Sciences (CAMS), and Tulane University in the United States. Key researchers of the study include Dr Li Liu and Professor Zhiwei Chen. Dr Liu is Research Assistant Professor in Department of Microbiology and the AIDS Institute; Professor Chen is Professor of Department of Microbiology and Director of the AIDS Institute, Li Ka Shing Faculty of Medicine, HKU. The institute focuses on viral mucosal pathogenesis and vaccine research.
Please visit the website at http://www.med.hku.hk/v1/news-and-events/press-releases for press photos.
Dr Li Liu, key researcher of the study, and Research Assistant Professor in Department of Microbiology and the AIDS Institute, Li Ka Shing Faculty of Medicine, HKU.