Media
HKU Discovered Mechanisms Underlying Fatal
SARS Acute Lung Injury
11 Mar 2019
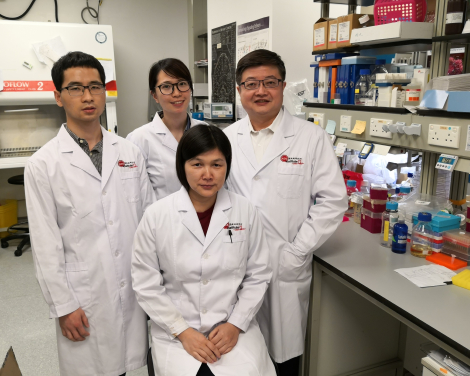
The research team led by scientists at AIDS Institute and Department of Microbiology, HKUMed (back row, from left): Mr Fang Jun, PhD student; Miss Maggie Kwok, Research Assistant; Professor Zhiwei Chen, Director of the AIDS Institute and Professor of Department of Microbiology; (front row) Dr Liu Li, Research Assistant Professor.
A research team led by scientists at AIDS Institute and Department of Microbiology, LKS Faculty of Medicine, The University of Hong Kong (HKUMed) discovered how host antibody response contributes to acute lung injury (ALI) during SARS-CoV infection. By adoptive transferring anti-SARS-CoV neutralizing antibody into Chinese macaques, the team found that purified anti-Spike IgG causes severe acute injury in infected lungs by skewing inflammation-resolving response. The new findings are now published in JCI Insight. (link to the publication)
Background
Severe acute respiratory syndrome coronavirus (SARS-CoV) causes fatal human respiratory disease. SARS patients displayed the characteristics of acute lung injury, including diffuse alveolar damage (DAD), epithelial necrosis, and fibrin and hyaline deposition. Patients who died of SARS developed acute respiratory distress syndrome (ARDS), the most severe form of ALI. Recent outbreaks of severe acute respiratory infections of emerging viruses, including Middle Eastern respiratory syndrome coronaviruses (MERS-CoV) and highly pathogenic avian influenza viruses (e.g., H5N1 and H7N9), highlight the need to investigate the mechanisms responsible for virus-mediated ALI or ARDS.
The team previously reported that the anti-SARS-CoV neutralizing-antibody (Nabs) response developed significantly faster in deceased patients compared to recovered patients after the onset of clinical symptoms. It took an average of 20 days for the recovered patients to reach their peak of Nab activities, as opposed to only 14.7 days for the deceased patients. Moreover, the actual Nab titer is significantly higher in deceased patients compared to that in the recovered patients during the same time period. These findings suggest a role of anti-S antibodies in ALI during SARS-CoV infection. Before the publication, the mechanism of virus-specific antibody response in SARS-CoV-induced ALI has not been previously investigated in vivo.
Research method and findings
The HKU research team constructed a vaccine using modified vaccinia Ankara (MVA) virus encoding full-length SARS-CoV S glycoprotein (ADS-MVA). They compared the pathological changes in the lungs of rhesus macaques vaccinated with ADS-MVA or control MVA at 7 and 35 days post pathogenic SARS-CoV challenge. They found significantly enhanced lung injury in ADS-MVA vaccinated group at both 7 and 35 dpi compared to control group, suggesting that S-specific but not MVA-specific immunity promotes ALI during SARS-CoV infection.
They then purified anti-Spike antibody (S-IgG) from the vaccinated macaques, and adoptively transferred the S-IgG and control IgG into groups of unvaccinated macaques via intravenous injection, respectively, and then intranasally challenged them with pathogenic SARS-CoV. They found that the presence of S-IgG at acute stage of SARS-CoV infection caused severe ALI. After analysing the lung tissue specimens from the macaques, they found that S-IgG inhibits macrophages’ inflammation-resolving response in the lungs during acute infection, resulted in increases in inflammatory cytokine/chemokine production, and enhanced inflammatory monocytes/macrohages infiltration and accumulation, and ALI. Notably, deceased SARS patients displayed similarly absence of macrophages’ inflammation-resolving response, accumulated pulmonary pro-inflammatory macrophages, and faster neutralizing-antibody responses. Their sera enhanced SARS-CoV-induced proinflammatory cytokine production by human monocytes-derived macrophages.
Therefore, the research team provides evidence that anti-SARS-CoV spike antibody causes severe ALI by skewing macrophage responses during acute SARS-CoV infection.
Significance of the study
Many newly emerging viruses, such as SARS-CoV in 2003, and MERS-CoV and H7N9 in recent outbreaks, cause fatal ALI by driving hypercytokinemia and aggressive inflammation in the lungs, however the mechanisms responsible for virus-mediated severe ALI remain elusive. The team’s findings reveal a mechanism responsible for virus-mediated ALI by defining the pathological role of viral specific antibody response. They also provide a potential target for treatment against SARS-CoV or other virus-mediated ALI.
About the research team
The HKU team is led by Professor Chen Zhiwei, Director of the AIDS Institute and Professor of Department of Microbiology, and conducted primarily by Research Assistant Professor Dr Liu Li. Three graduate students Mr Lin Qingqing, Mr Fang Jun, Dr Peng Jie, and two Research Assistant Ms Kwok Hauyee and Ms Tang Hangying made important contributions. Key internal collaborators include Professor Yuen Kwok-yung and Dr Chan Kwokhung of Department of Microbiology, HKUMed. Key external collaborators include Professors Wei Qiang and Chuan Qin at Institute of Laboratory Animal Science, Chinese Academy of Medical Sciences, Dr Xavier Alvarez and Professor Andrew Lackner at Tulane National Primate Research Center (TNPRC), and Stanley Perlman at University of Iowa.
The work was supported by the grants from the US National Institutes of Health (RO1HL080211) and HK Research Grants Council (TRS T11-706/18-N to ZC), the Tulane National Primate Research Center (base grant RR00164), the Health and Medical Research Fund (16150662), and the University Development Fund/Li Ka Shing Faculty of Medicine Matching Fund of The University of Hong Kong to its AIDS Institute.
Media enquiries
Please contact LKS Faculty of Medicine of The University of Hong Kong by email (medkefa@hku.hk).
Please visit the website at http://www.med.hku.hk/news/ for press photo and presentation slides.