Media
HKUMed researchers reveal benefits of Tai Chi
in reducing central obesity
30 Jul 2021
HKUMed researchers at the School of Public Health, LKS Faculty of Medicine at The University of Hong Kong (HKUMed) and collaborators from The Chinese University of Hong Kong, the Chinese Academy of Sciences, and the University of California, Los Angeles (UCLA) have found that Tai Chi mirrors the benefits of conventional exercise in reducing waist circumference of older adults with central (abdominal) obesity1. The findings are now published in Annals of Internal Medicine [link to the publication].
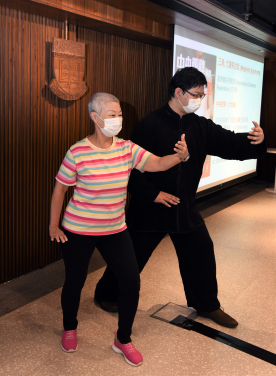
Tai Chi (officially named T’ai chi ch’üan or Taijiquan) is a centuries-old Chinese martial art and an ancient form of mind-body exercise, often described as the ‘meditation in motion’. In 2020, it was added to the United Nations Educational, Scientific and Cultural Organization (UNESCO) representative list of intangible cultural heritage of humanity. As a low-impact and moderate-intensity exercise, Tai Chi is known to be suitable for older adults2, including those who are inactive or with limited mobility. However, there has been little rigorous scientific evidence on Tai Chi’s metabolic health benefits in people with central obesity.
Between February 2016 and March 2018, 543 Chinese adults over 50 years of age with central obesity were enrolled and randomly assigned to a regimen of Tai Chi, conventional exercise, or no exercise. Participants in the Tai Chi and conventional exercise groups were required to meet for a one-hour instructor-led workout three times a week for 12 weeks. For the Tai Chi group, the 24-form Yang style, recognised as the most commonly practised style, was adopted. For the conventional exercise group, brisk walking and muscle-strengthening activities such as arm curl and raise, shoulder press, squats and heel raise were performed.
Waist circumference and other indicators of metabolic health of all the participants were measured before the programme began (baseline), week 12, and week 38. It was found that, without any dietary intervention, both the Tai Chi and conventional exercise groups had an average reduction of 1.8 cm and 1.3 cm in waist circumference at week 12 respectively, compared to the control group. The interventions also had a favourable impact on HDL cholesterol, or so-called ‘good cholesterol’. While the HDL cholesterol levels of the control group continued to decline from 1.51 mmol/L to 1.41 mmol/L over time, both the Tai Chi and conventional exercise groups could maintain a higher level of HDL cholesterol at 1.52 mmol/L or above even at week 38. But the study did not show detectable differences in fasting glucose or blood pressure among the three groups.
‘Recent recommendations3 have suggested that waist circumference (WC) is considered an important factor for risk factors associated with overweight, including Type 2 diabetes and cardiovascular disease, partly because Asians generally have a higher body fat percentage than Caucasians of the same age, sex and body mass index (BMI). This was one of the factors that inspired us to identify effective ways of reducing WC to prevent obesity,’ said Dr Parco Siu Ming-fai, Associate Professor and Division Head of Kinesiology, School of Public Health, HKUMed.
‘Our research showed that Tai Chi can be an effective alternative to conventional exercise in the management of central obesity. This is good news for older people with central obesity who may be averse to conventional exercise due to preference or limited mobility. However, further research is needed to reveal how the identified health benefits are achieved through Tai Chi,’ Dr Siu added.
About the research team
The research was conducted by Dr Parco Siu Ming-fai, Associate Professor and Division Head of Kinesiology; Mr Angus Yu Pak-hung and Mr Edwin Chin Chun-yip, PhD students, School of Public Health, HKUMed; Dr Daniel Fong Yee-tak, Associate Professor and Professor Doris Yu Sau-fung, Professor at School of Nursing, HKUMed; Professor Stanley Hui Sai-chuen and Professor Jean Woo Ling-fong, The Chinese University of Hong Kong; Dr Wei Gaoxia, the Chinese Academy of Sciences; and Professor Michael Irwin, UCLA.
This project was supported by the Health and Medical Research Fund (Grant no. 12131841), Food and Health Bureau, Government of the Hong Kong Special Administrative Region.
About the School of Public Health, HKUMed
The School of Public Health, LKS Faculty of Medicine of The University of Hong Kong has a long and distinguished history in public health education and high impact research. With world leading research in infectious diseases as well as on non-communicable diseases of both local and global importance, the School has made significant contributions through its research and advocacy to improve the health of populations and individuals, both locally and globally. The School is a leading research and teaching hub in public health on influenza and other emerging viruses, control of non-communicable and infectious diseases, tobacco control, air pollution, psycho-oncology, behavioural sciences, exercise science, life-course epidemiology, and health economics, health services planning and management. This work has informed international (e.g. the US Food and Drug Administration, Health Canada, the World Health Organization), national and local public health policies.
Media enquiries
Please contact LKS Faculty of Medicine of The University of Hong Kong by email (medmedia@hku.hk).
1For most Asian adults including Chinese, central obesity is defined if waist circumference is ≥ 90 cm (35.5 inches) for men, and ≥ 80 cm (31.5 inches) for women. The Asia-Pacific Perspective: Redefining Obesity and its Treatment. Geneva: World Health Organization, 2000.
2Wang C, Collet JP, Lau J. The effect of Tai Chi on health outcomes in patients with chronic conditions: a systematic review. Arch Intern Med. 2004 Mar 8;164(5):493-501. doi: 10.1001/archinte.164.5.493.
3Ross R, Neeland IJ, Yamashita S, et al. Waist circumference as a vital sign in clinical practice: a consensus statement from the IAS and ICCR Working Group on Visceral Obesity. Nat Rev Endocrinol. 2020;16:177-89.