Media
HKU Dentistry study finds facial asymmetry correction surgery effective
in relieving syndrome of jaw joint pain patients
14 Nov 2021
Jaw joint pain, or clinically known as temporomandibular disorder (TMD), affects the jaw muscles and joints. The known prevalence of TMDs is around 5% to 12% in the general population globally. TMD patients will experience discomfort or even pain at jaw joint areas when they eat, talk or open their mouths. TMDs are known to be associated with depression and mood disorders.
In a recent study, an Oral and Maxillofacial Surgery (OMFS) research team at the Faculty of Dentistry of the University of Hong Kong (HKU) revealed that jaw asymmetry is likely to be a causative factor of jaw joint pain, and that surgical correction of facial asymmetry is effective in improving or even curing patients suffering from jaw joint pain.
The research team led by Clinical Associate Professor in OMFS Dr Mike YY Leung, with Dr Aileen Toh as co-investigator, has published the findings in an article titled “Mandibular asymmetry as a possible etiopathologic factor in temporomandibular disorder: a prospective cohort of 134 patients” in academic journal Clinical Oral Investigations.
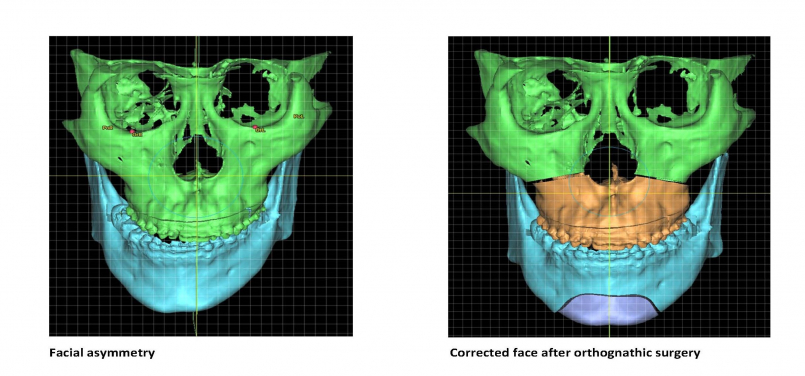
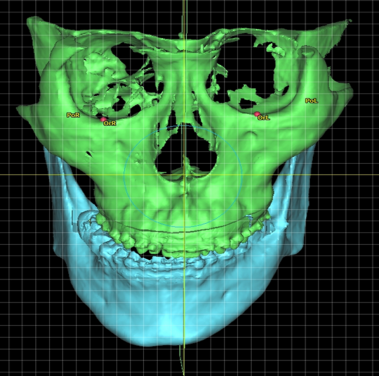
Facial asymmetry can be a result of the difference in jaws’ growth rate or caused by trauma. Patients with facial asymmetry will see a difference in the length of the left and right side of the jaws, which result in a deviated face as well as a shifted bite. The asymmetric face not only affects the facial appearance of the individual, but also hinders the eating or speech function and lowers the patient’s self-esteem.
Jaw correction surgery, or orthognathic surgery, is the surgical treatment for patients with dentofacial deformities including facial asymmetry. In the surgery, the deformed jaws are surgically corrected in a planned and normalized position so as to improve the patient’s masticatory and speech function, as well as symmetry and facial profile. It is a routine procedure performed by OMFS surgeons and will usually take three to six weeks to recover.
In the study, Dr Leung’s team investigated the prevalence of TMDs in 134 patients. Among them, 82 were with facial asymmetry while 52 with other facial deformities without asymmetry.
It was found that the prevalence of TMD in patients with facial asymmetry was 67.1%, which was significantly higher than those without (40.4%). Of these patients with facial asymmetry, 78.2% are presented with temporomandibular joint (the joint which connects the lower jaw to the skull) (TMJ) disc displacement with reduction, 34.5% have myalgia (muscle pain), and 20% have arthralgia (joint pain) (Note 1). The study shows that patients with dentofacial deformity, in particular facial asymmetry, are much more likely to suffer from TMD than individuals without such deformity.
Since the result suggests TMD could be caused by facial asymmetry, the research team further investigated the effect of orthognathic surgery to correct facial asymmetry and the prevalence of TMD. It was found that the prevalence of TMD in patients with facial asymmetry who underwent jaw correction surgery has reduced by 58.3% at 6 months after the surgery. The finding indicates that surgical correction of facial asymmetry is effective in improving or even curing TMD in these patients.
“We believe patients with facial asymmetry have an imbalanced force to the jaw joints and the masticatory muscles. This may induce chronic trauma to the TMJ and the musculature system in the long-term, which explained the high prevalence of TMD-related symptoms including pain and limited mouth opening in this group.” Dr Aileen Toh said.
“The surgical correction of facial asymmetry allows a normalised masticatory function and a corrected bite, and now we prove it also helps in treating TMDs. Many people misunderstood orthognathic surgery is for aesthetic reasons, in fact the correction of a facial deformity improves the sufferer’s function as well as reduces pain symptoms as a consequence of TMDs.” Dr Mike Leung added.
The research team will further look into the long-term effect of the surgical treatment on TMD and if any relapse will occur.
Note 1: Patients may have more than one symptoms
Journal: Clinical Oral Investigations 2021 July; 25, pages4445–4450.Mandibular asymmetry as a possible etiopathologic factor in temporomandibular disorder: a prospective cohort of 134 patients. Aileen Qiu Jin Toh, Joshua Lue Hang Chan, Yiu Yan Leung. (Link: https://link.springer.com/article/10.1007%2Fs00784-020-03756-w)
For enquiries, please contact:
Ms Melody Tang, Senior Communications Officer of the Faculty of Dentistry, HKU
Tel: 2859 0494 / 9155 0980
Email:meltang@hku.hk